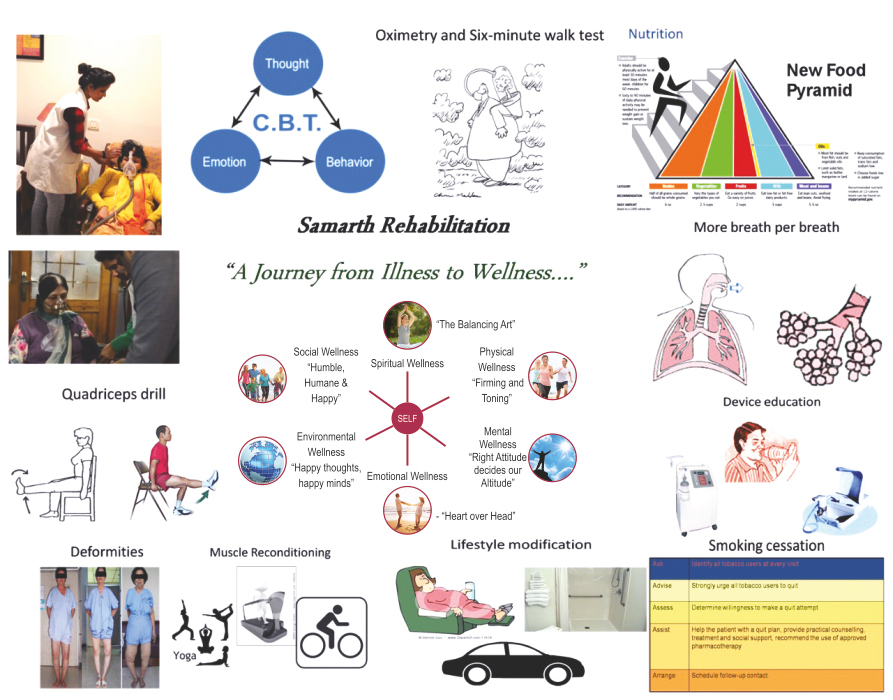
"A Journey from Illness to Wellness"
Pulmonary Rehab Algorithm


Key Points

Components of a Comprehensive Program
- Assessment
- Education
- Exercise Training
- Psychosocial/Behavioral intervention
- Nutrition
- Breathing techniques
- Medications, devices & specific therapy
- Outcome Assessment
Rehabilitation tries to address morbidities and their consequences through education and exercise. Patients are encouraged to become more actively involved in their own health care, more independent in ADLs and less dependent on health professionals and expensive medical resources. Rather than focusing solely on reversing disease processes, rehab attempts to reduce symptoms and make individual more functional
Purpose
Restore function following an illness or injury, with the goal of maximizing a person’s ability to achieve fullest life possible
- Chronic respiratory disease symptomatic with optimum drug therapy
- Chronic cardiovascular diseases with breathlessness despite optimum intervention and drug therapy
- Chronic neurological diseases
- Chronic orthopaedic diseases & post-operative
- Lifestyle disorders like Stress,Sleep, Obesity
- Special children
- Deconditioning
- Malnutrition
- Effects of hypoxemia
- Steroid myopathy
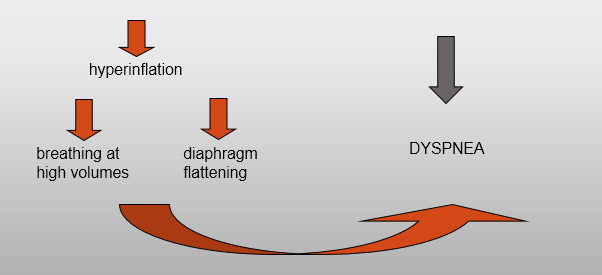
- Hyperinflation
- Diaphragmatic fatigue
- Psychosocial dysfunction from anxiety, guilt, dependency and sleep disturbances.
- Peripheral Muscle dysfunction
- Respiratory muscle dysfunction
- Nutritional abnormalities
- Cardiac impairment
- Skeletal disease
- Sensory defects
- Neurocognitive dysfunction
- Psychosocial dysfunction
- Improved Exercise Capacity
- Reduced perceived intensity of dyspnea
- Improve health-related QOL
- Reduced hospitalization
- Reduced anxiety and depression
- Improved limb function
- Benefits extend well beyond the immediate period of training.
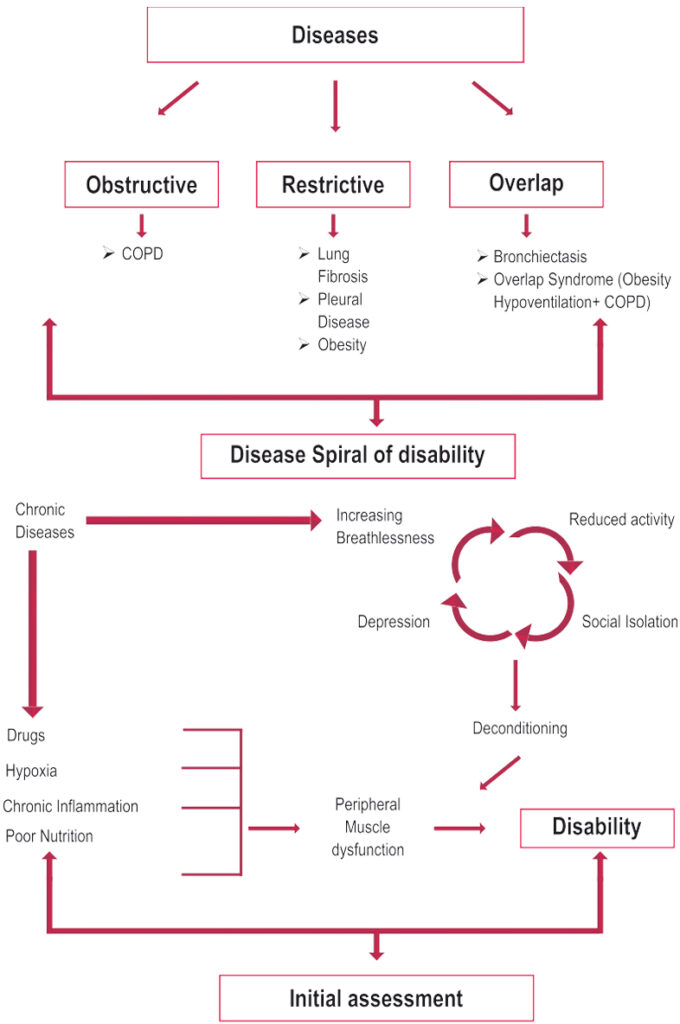
Causes of Dyspnea in COPD
narrowed airways (bronchospasm, increased compliance airway secretions, airway thickening, increased cholinergic tone)
- Peripheral Muscle dysfunction
- Respiratory muscle dysfunction
- Nutritional abnormalities
- Cardiac impairment
- Skeletal disease
- Sensory defects
- Psychosocial dysfunction
- Deconditioning
- Malnutrition
- Effects of hypoxemia
- Steroid myopathy or ICU neuropathy
- Hyperinflation
- Diaphragmatic fatigue
- Psychosocial dysfunction from anxiety, guilt, dependency and sleep disturbances.
Pulmonary Rehabilitation
“A multidisciplinary continuum of services directed to persons with pulmonary diseases and their families, usually by an interdisciplinary team of specialists, with the goal of achieving and maintaining the individual’s maximum level of independence and functioning in the community”
Benefits of Pulmonary Rehab
The benefits are seen in irreversible pulmonary disorders because much of the disability is not from the lung disease but from the secondary morbidities.
- FEV1 less than 80% predicted
- FEV1/FVC less than 70 %
- DLCO less than or equal to 65% of predicted
- Resting hypoxemia less than or equal to 90%
- Exercise Testing demonstrating hypoxemia less than 90%
- Enrolling active smokers is controversial but they may benefit significantly with a focus on smoking cessation.
- Patient Motivation is a necessary consideration.
- Exercise Training
- Education
- Medication and other therapies
- Psychosocial/behavioural intervention
- Chest – physical therapy
- Nutrition assessment
- Outcome Assessment
- Diet history, BMI
- Over or Under weight.
- Classes in weight management and/or nutritional counseling to improve weight management
- Outpatient
- Inpatient
- Home
- Community-Based
- Choice varies depending on
- Distance to program
- Insurance payer coverage
- Patient preference
- Physical, functional, psychosocial status of patient
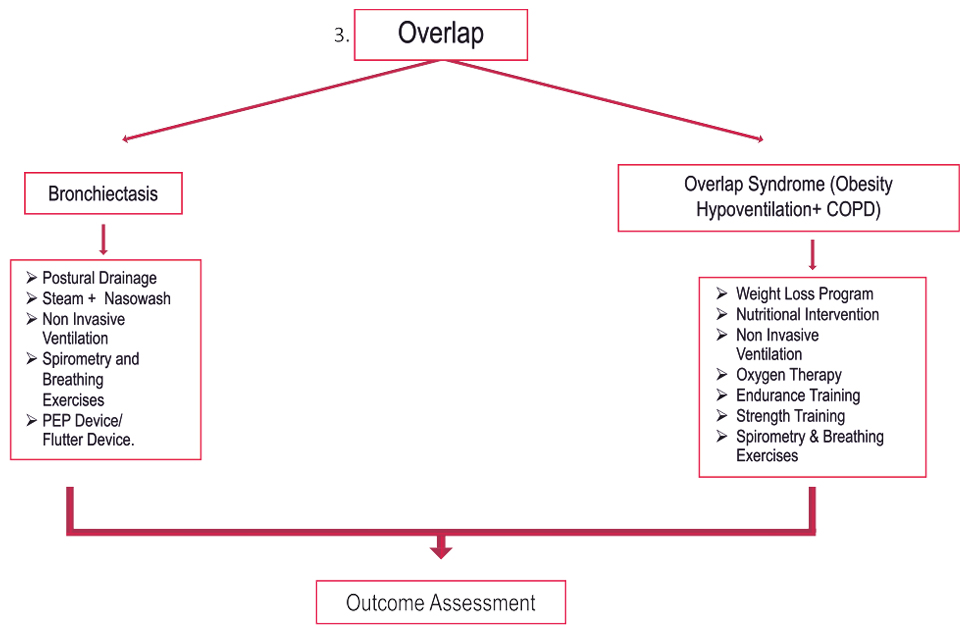
- Pursed Lip Breathing – shifts breathing pattern and inhibits dynamic airway collapse.
- Posture techniques – forward leaning reduces respiratory effort, elevating depressed diaphragm by shifting abdominal contents.
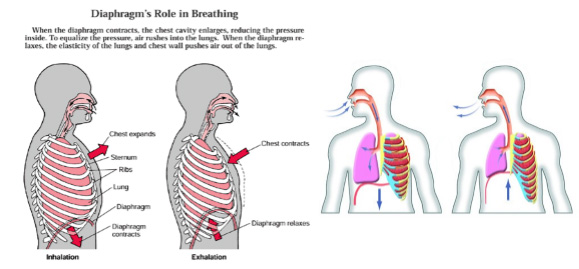
- Diaphragm Breathing – Some patients with extreme air trapping and hyperinflation have increased WOB with this technique
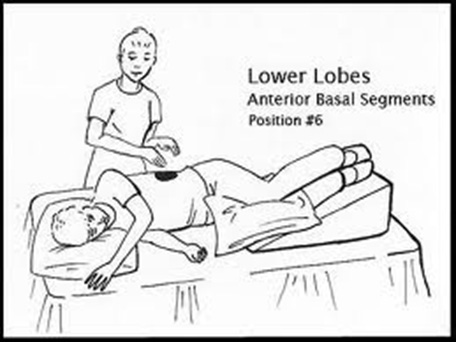
- Postural Draining – valuable in patients who produce more than 30cc/24 hours/ Coughing techniques
- An important component of pulmonary rehabilitation, is used to determine individual patient responses and evaluate the overall effectiveness of the program.
- Dyspnea 10 pt scale, Borg scale, Visual Analog Scale
- Exercise Ability – Borg Scale, 6MDW/Progressive exercise testing pre and post-rehab.
- Health Status – Respiratory-related QOL; CRDQ
- Activity Levels –Respiratory-Specific functional Status, Duke Functional Status Scale.
Quit Smoking


Motivation

Quit Smoking
Pursed lip breathing

Diaphragmatic breathing
Mucus clearing and postural drainage
Device education

Oximetry and Six-minute walk test

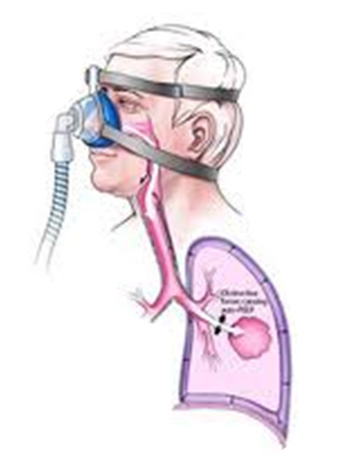
Non-invasive ventilation